Blood Volume in Hemodialysis & Treatment of Kidney Failure
What is Kidney Disease?
Kidney disease, or renal disease is damage to or disease of a kidney. Kidney disease usually causes a loss of kidney function and can result in kidney failure. Kidney failure is known as the end-stage of kidney disease, where dialysis or a kidney transplant is the only treatment option.
Kidney failure can be divided into acute kidney failure or chronic kidney failure (CKD). While acute kidney failure is often reversible chronic kidney failure is not. Causes of CKD include diabetes, high blood pressure, nephrotic syndrome, and polycystic kidney disease. Complications with CKD include uremia, high blood pressure, fluid, and volume overload as well as heart disease and anemia.

Benefits of Blood Volume Guided Treatment for Kidney Failure
Research on Blood Volume Guided Treatment
Researchers ways, by hemodialysis, to remove what blood volume is in excess corresponding to normal values. Researchers speculate that blood volume-guided hemodialysis could optimize the volume that may be removed per dialysis so that procedures performed per week could be reduced. Studies have shown that the risk of developing intradialytic hypotension following hemodialysis is high (15-30%). This is unfortunate as intradialytic hypotension is associated with several severe consequences for the patient.
Healthy kidneys produce the hormone erythropoietin that stimulates the bone marrow to produce red blood cells. As the kidneys fail, they may produce less erythropoietin, resulting in decreased production of red blood cells which will eventually lead to anemia. Hence, many chronic kidney failure patients are being treated with recombinant human erythropoietin. As many chronic kidney failure patients may also be volume overloaded, (i.e. expanded plasma volume) it can be difficult to diagnose if an anemic CKD patient should receive erythropoietin treatment or not. However, blood volume measurement is now a good clinical solution to that problem.
Researchers using the Detalo blood volume measurement devices have documented that out of 26 anemic CKD patients, 14 were in fact dilutional anemic due to hypervolemia and did not lack red blood cells.

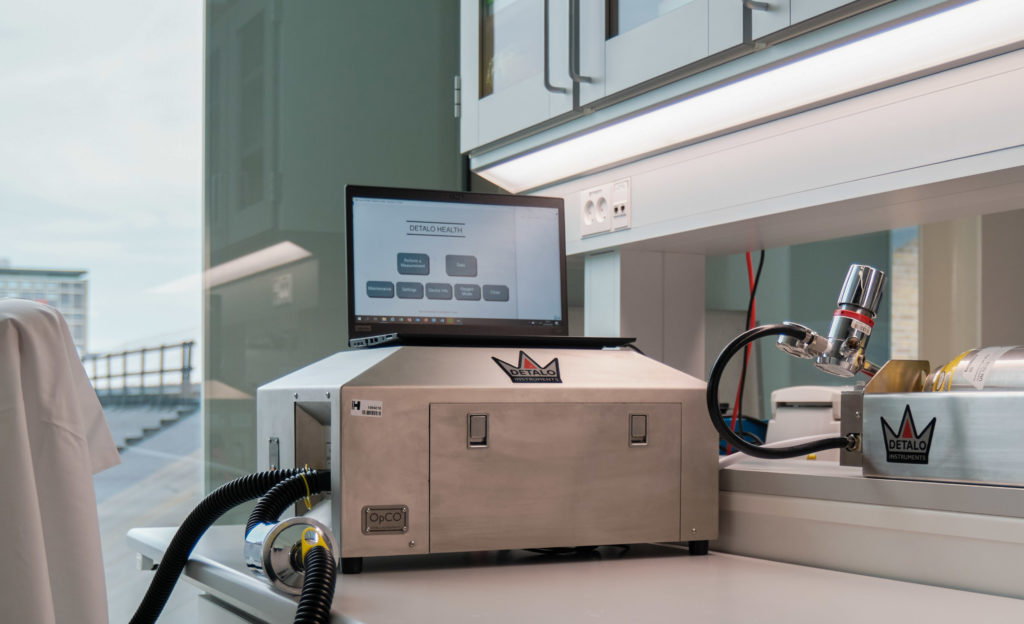
Blood Volume Measurement in 15 Minutes
Detalo blood volume analyzers determine total blood volume, red blood cell volume, and plasma volume in humans in a rapid, safe, and precise manner.
The Detalo Clinical™ is a CE-certified (MDR) medical device for routine blood volume assessment in standard clinical care. The device allows healthcare professionals to distinguish between true anemia and dilutional anemia and to determine if a patient is euvolemic, hypovolemic, or hypervolemic. Finally, it allows clinicians to evaluate and track the effectiveness of a treatment intended to change blood volume.